Healthcare supply chains rarely make headlines. Yet they decide whether a hospital has the right implant at the right moment or whether a life-saving drug reaches a patient on time. Over the past few years, cracks in this system have become impossible to ignore.
Cost pressure, workforce shortages, global disruptions, and rising patient expectations are forcing healthcare leaders to rethink how supply chains actually work. What follows are ten trends that are quietly, but decisively, changing the way healthcare supply chains operate.
1. Visibility is no longer optional
Hospitals are moving away from guesswork. Leaders want real-time clarity on what they have, where it is, and how fast it moves. Without visibility, waste hides in plain sight. Overstocked shelves coexist with urgent shortages. Digital tracking tools, dashboards, and connected inventory systems are now seen as operational necessities, not upgrades.
2. Data-driven forecasting replaces intuition
For decades, ordering decisions relied on experience and habit. That approach is fading. Advanced analytics now help predict demand based on historical usage, seasonal patterns, and procedure schedules. This shift reduces last-minute orders and cuts excess inventory, which directly impacts cash flow and patient readiness.
3. Inventory management becomes clinical
Supplies are no longer treated as generic stock. High-value items like implants, surgical kits, and critical drugs are managed with the same seriousness as clinical assets. This is where RFID hospital inventory management earns attention, especially for reducing loss, expiry-related waste, and manual counting errors.
4. Resilience over pure cost savings
The lowest-cost supplier is no longer the safest bet. Healthcare organizations are diversifying vendors and building contingency plans. Short-term savings mean little if a disruption delays surgeries or compromises patient care. Reliability and continuity now weigh just as heavily as price.
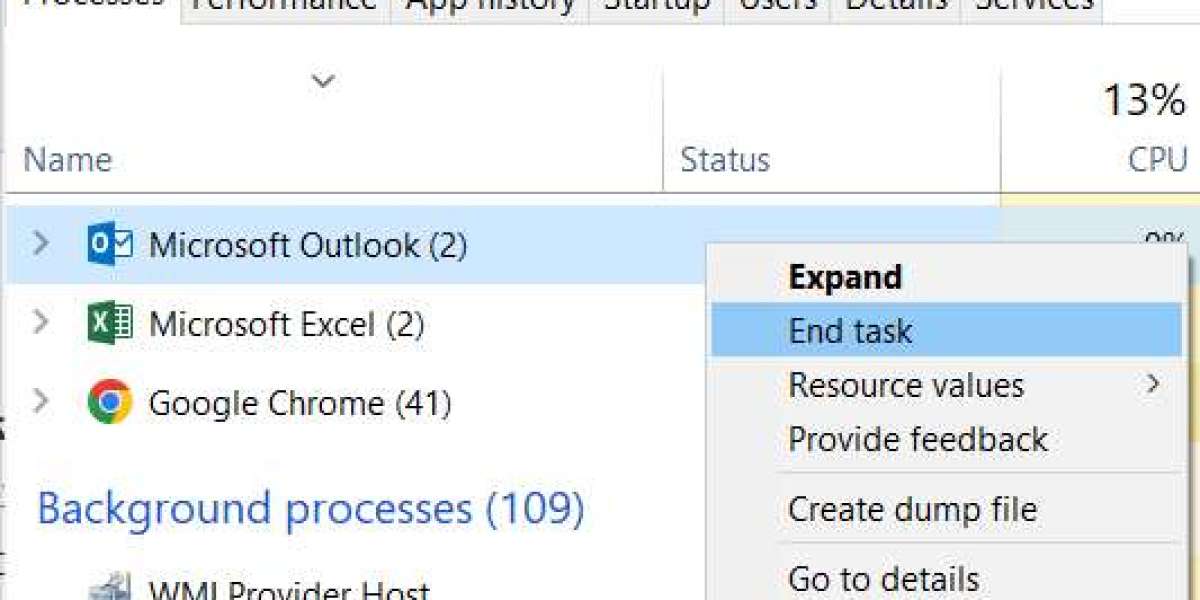
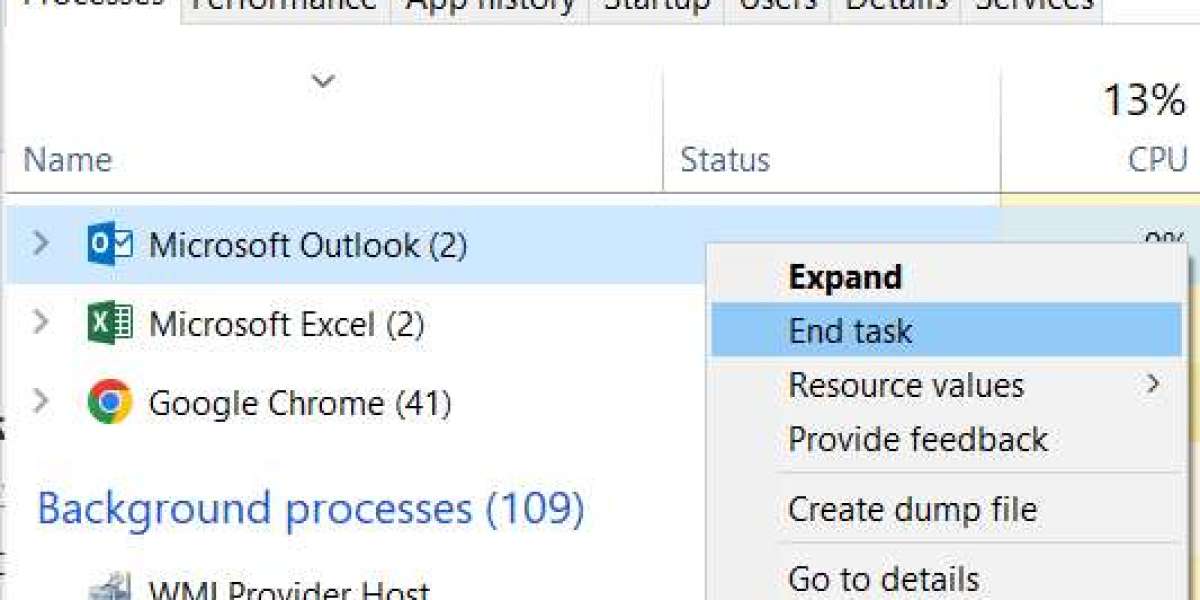
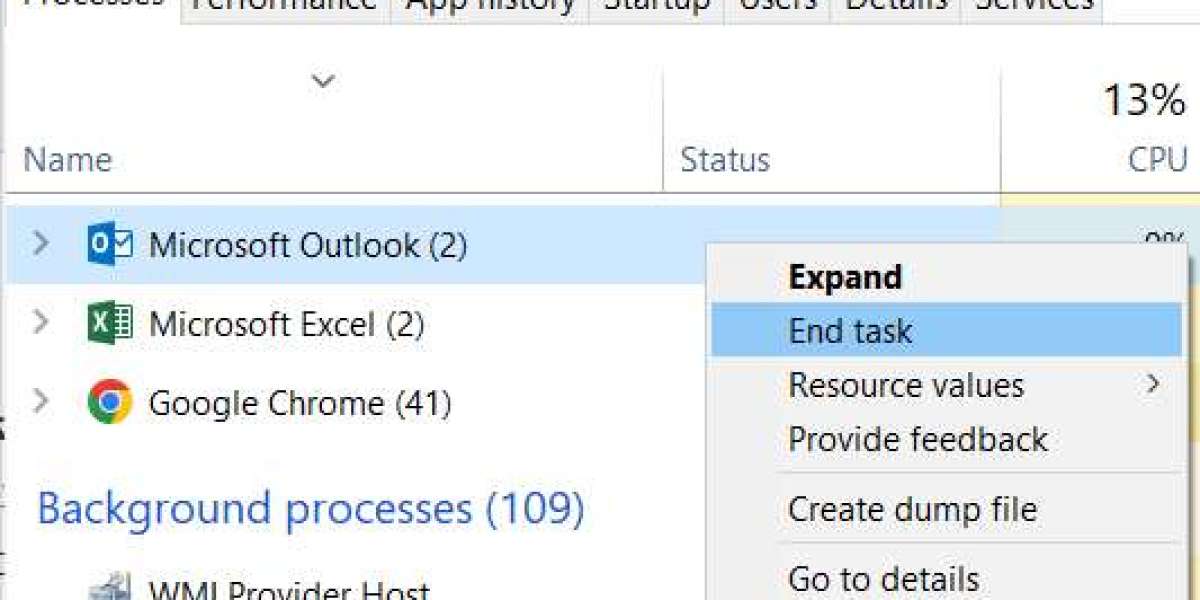
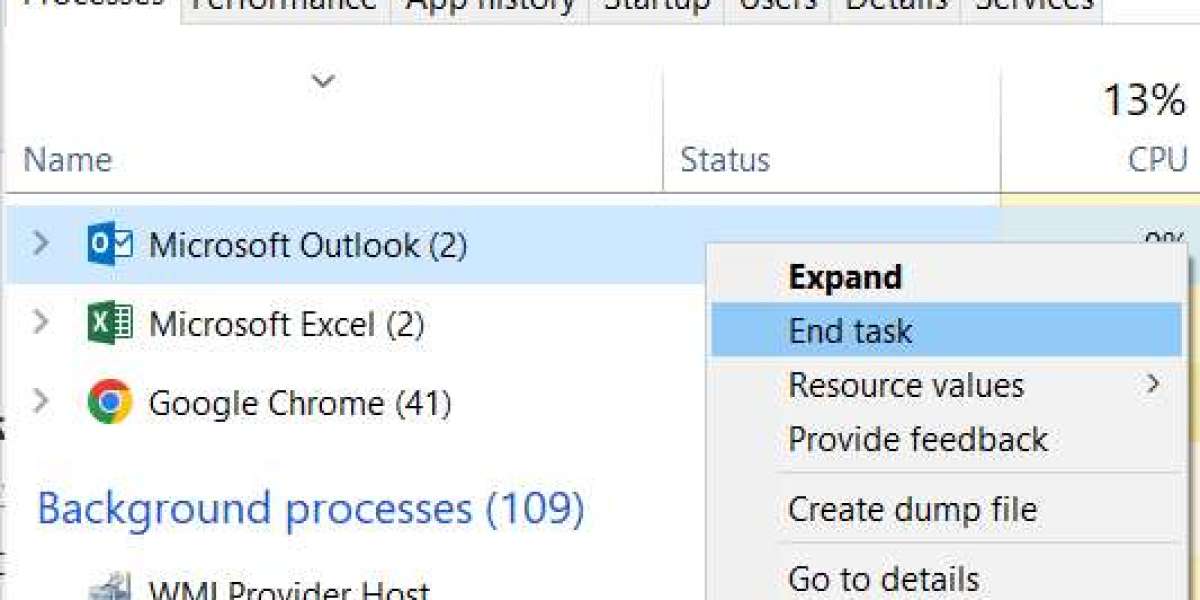
5. Automation enters everyday operations
Manual processes slow teams down. Automated replenishment, barcode scanning, and system-driven reorder points free staff to focus on patient-facing work. Automation also reduces fatigue-related errors, a quiet but serious issue in high-pressure hospital environments.
6. Sustainability moves into procurement decisions
Healthcare generates significant waste. Supply chain leaders are under pressure to choose suppliers with sustainable packaging, ethical sourcing, and lower environmental impact. This is no longer about branding. It affects compliance, community trust, and long-term operational costs.
7. Integration across departments improves flow
Supply chain, finance, and clinical teams are beginning to work from shared systems instead of silos. When procurement data connects directly to billing and usage records, discrepancies shrink. This integration also supports better auditing and regulatory reporting.
8. Local sourcing gains renewed importance
Global suppliers still matter, but many healthcare systems are strengthening local partnerships. Shorter supply routes mean faster response times and reduced dependency on international shipping. The pandemic accelerated this mindset, and it has not reversed.
9. Lessons from retail logistics influence healthcare
Healthcare is borrowing operational discipline from other sectors without copying their models blindly. Concepts such as demand smoothing, just-in-time delivery, and shelf-level tracking—often discussed in the context of RFID retail—are being carefully adapted to clinical realities where patient safety comes first.
10. Talent and training become strategic priorities
Technology alone does not fix supply chains. Skilled professionals who understand data, compliance, and clinical needs are in short supply. Hospitals are investing in training programs and redefining supply chain roles to attract and retain capable teams.
.jpg)
Why do these trends matter now?
These changes are not theoretical. They affect operating margins, staff workload, and patient outcomes every single day. Healthcare organizations that adapt early tend to gain stability and trust. Those who delay often pay more later, both financially and reputationally.