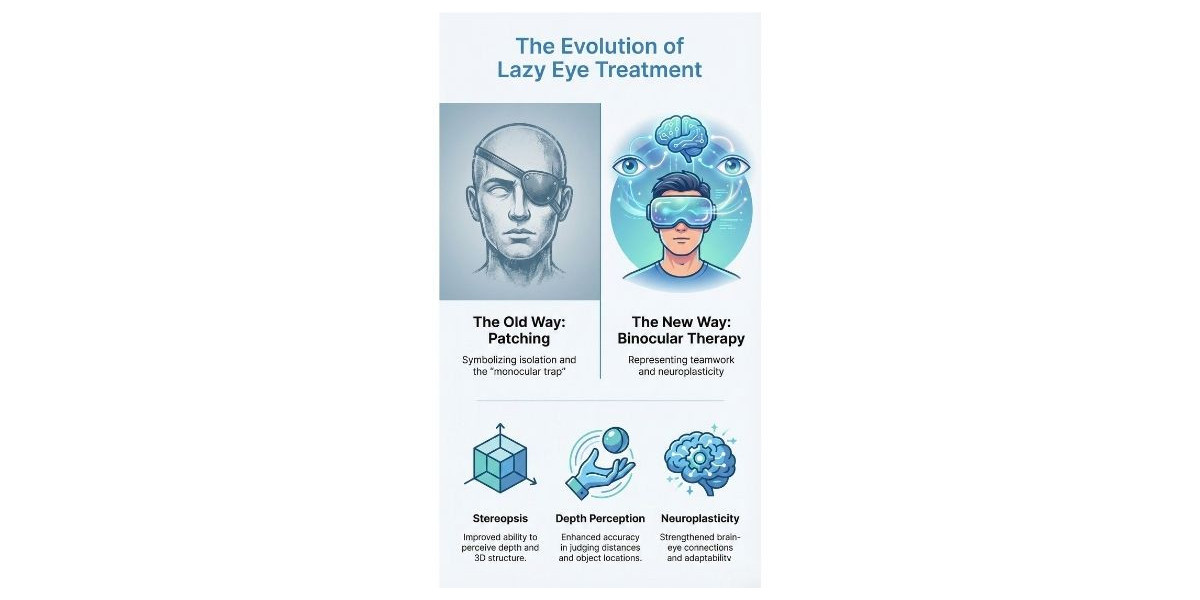
Imagine trying to learn how to clap with one hand tied behind your back. You might make your free hand stronger, but you aren't teaching your hands how to work together. For a long time, this was essentially how we approached one of the most common vision disorders in the world. If you or your child has been diagnosed with amblyopia, you are likely familiar with the pirate patch. It is the classic symbol of vision correction, a method that has been around for centuries.
For generations, the go-to advice has been simple: cover the strong eye to force the weak one to work. While this lazy eye treatment has helped many, it often overlooks a crucial piece of the puzzle: how the two eyes work together as a team. The landscape of vision care is shifting, moving away from isolation and toward coordination. We are discovering that the key to lasting visual improvement isn't just about making one eye stronger—it is about teaching the brain to use both eyes simultaneously.
The "Good Eye" Trap: Understanding the Limitations
To understand why modern science is looking beyond the patch, we first have to understand the condition itself. Amblyopia is not just an issue of "weak" muscles or a "lazy" eye; it is a neurological disconnect. The brain, receiving a blurry or conflicting image from one eye, decides to ignore that input to avoid confusion (like double vision). It creates a suppression zone, relying entirely on the "good" eye.
Traditional patching falls into what experts call the "monocular" trap. By covering the dominant eye, we force the brain to pay attention to the weaker eye. While this often improves visual acuity (the ability to read letters on a chart) in the short term, it doesn't solve the underlying rivalry between the eyes.
When the patch comes off, the brain often reverts to its old habit. It remembers that it is easier to just use the strong eye, and the suppression returns. This is why some patients see their vision regress after they stop patching. They improved the strength of the isolated eye, but they never learned binocular vision—the ability to fuse images from both eyes into a single, 3D picture.
It’s A Brain Problem, Not Just an Eye Problem
The most exciting developments in vision science come from understanding that we see with our brains, not just our eyes. The eyes are merely the cameras; the visual cortex is the processor.
In cases of amblyopia, the hardware (the eye) might be capable of seeing, but the software (the brain) is actively blocking the signal. This is where the concept of neuroplasticity comes into play. Neuroplasticity is the brain's incredible ability to rewire itself, form new connections, and adapt to new information.
For a long time, it was believed that this window of opportunity closed after childhood (usually around age 7 or 8). We now know that the brain remains plastic well into adulthood. This discovery has paved the way for new therapies that target the brain's processing power rather than just the eye's focusing ability.
Beyond the Patch: The Rise of Binocular Therapy
If patching is like lifting weights with one arm, modern lazy eye treatment is like learning to juggle. It focuses on coordination and cooperation. This approach is often referred to as dichoptic therapy.
The premise is simple yet revolutionary: instead of blocking the strong eye completely, why not dim its input just enough so the weak eye can participate?
How Digital Therapy Works
Modern solutions often utilize digital platforms, video games, and virtual reality environments to create a balanced visual experience. Here is how it generally works:
Contrast Balancing: The system presents a game or video. The strong eye sees a version of the image with lower contrast (dimmer), while the weaker eye sees a high-contrast (brighter) version.
The "Pop-Out" Effect: Because the image is brighter for the weaker eye, the brain is encouraged to pay attention to it.
Simultaneous Use: Since the strong eye isn't covered, the brain learns to keep both channels open. It starts fusing the two images to play the game effectively.
This method transforms therapy from a passive chore into an active, engaging process. Instead of struggling with a patch at school or work, patients play specialized games that reward them for using both eyes together. This active engagement triggers neuroplastic changes faster and more effectively than passive occlusion.
Why "Teamwork" is Better Than Strength
When the eyes learn to work as a team, the benefits extend far beyond just reading lines on a chart. True binocular vision unlocks a different way of experiencing the world.
Stereopsis (3D Vision): This is the ability to judge depth accurately. It is essential for catching a ball, driving, parking, or even pouring water into a glass without spilling.
Wider Field of View: Using both eyes provides a fuller picture of your surroundings.
Faster Processing: Two eyes feed information to the brain faster than one, improving reaction times.
By focusing on binocularity, modern therapies aim to restore these functional skills, improving the quality of life in ways that simple acuity improvements cannot.
Can Adults Benefit? Busting the Age Myth
One of the most persistent myths in optometry is that if you didn't fix a lazy eye by age seven, you were out of luck. This outdated belief left millions of adults thinking there was no hope for their vision.
Thanks to our understanding of adult neuroplasticity, we now know this is false. While the adult brain might take a little longer to rewire than a child's, it is entirely capable of change. Digital, binocular therapies have shown remarkable success in adults, improving visual acuity and depth perception in patients who had given up hope years ago. Fortunately, effective lazy eye treatment is no longer limited to just early childhood.
Signs You or Your Child Might Need Support
Amblyopia isn't always obvious. There isn't always a visible "turn" or squint. Because the brain is so good at compensating with the strong eye, children (and adults) often don't realize they aren't seeing the world as clearly as they could be.
Here are some common signs that might indicate a binocular vision disorder:
Clumsiness: Frequently bumping into furniture or knocking things over.
Poor Hand-Eye Coordination: Difficulty catching or hitting a ball.
Head Tilting: Tilting the head to one side to see better or watch TV.
Squinting: Closing one eye in bright sunlight or when reading.
Eye Strain: Frequent complaints of tired eyes or headaches, especially after screen time.
Difficulty Reading: Skipping lines or losing place on the page.
Why Early Diagnosis Still Matters
While we have established that it is never too late to treat amblyopia, early detection remains the gold standard. The sooner a diagnosis is made, the faster the brain can be retrained.
Pediatric eye exams are crucial because children rarely complain about vision problems—they assume everyone sees the way they do. Catching the issue early prevents the brain from solidifying those suppression pathways, making the journey to full binocular vision smoother and faster.
However, if you missed that early window, take heart. The science has evolved. The "Good Eye" trap is no longer the only option. With the advent of digital, brain-based therapies, we are moving toward a future where eyes are treated not as solo players, but as the dynamic team they were meant to be.
Conclusion
The journey to better vision is evolving. We are moving away from the era of simply covering the strong eye and hoping for the best. The future lies in engaging the brain, utilizing advanced technology, and fostering true cooperation between the eyes. By understanding that vision is a neurological process, we open the door to more effective, comfortable, and lasting solutions. Whether for a child struggling in school or an adult looking to improve their depth perception, the shift toward binocular therapy offers a new perspective on what is possible for eye health.
Frequently Asked Questions
1. Is eye patching completely outdated?
Not necessarily. Patching is still a valid and widely used method, especially for very young children. However, many experts now view it as part of a broader toolkit rather than the only solution. It is often most effective when combined with activities that encourage the eyes to work together.
2. Can digital vision therapy replace surgery?
Therapy and surgery address different issues. Surgery is typically used to correct the physical alignment of the muscles (strabismus). However, surgery doesn't always teach the brain to use the eyes together. Vision therapy is often recommended before or after surgery to retrain the brain and ensure functional binocular vision.
3. How long does it take to see results with modern therapy?
Every case is unique, depending on the severity of the condition and the patient's compliance. However, because digital therapies are active and engaging, many patients report noticing improvements in weeks rather than the years often associated with traditional methods.
4. Is this type of therapy suitable for adults?
Yes. Modern research into neuroplasticity has proven that the adult brain can learn and adapt. Many adults have successfully improved their depth perception and visual acuity through binocular vision training.
5. Do I need special equipment for these new treatments?
Most modern programs are designed to be convenient. They often utilize standard computers or tablets, sometimes paired with specialized glasses (like red-blue or VR headsets) provided by the vision care professional to create the dichoptic effect.