A crucial phase in the healthcare process is prior authorization, which guarantees that insurers approve operations, treatments, and prescription drugs prior to delivery. However, the provider prior permission procedure has long been a cause of inefficiencies, delays, and administrative strain. These days, automation systems are changing this environment by assisting clinics in improving patient care and streamlining procedures.
Simplifying the Flow of the Healthcare Prior Authorization Process
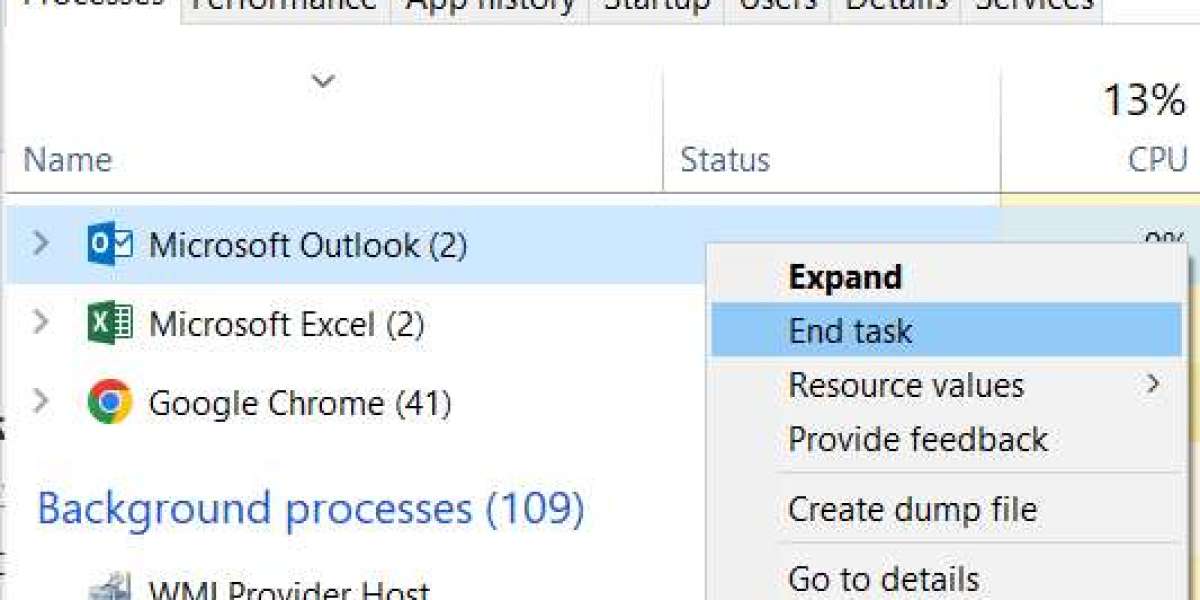
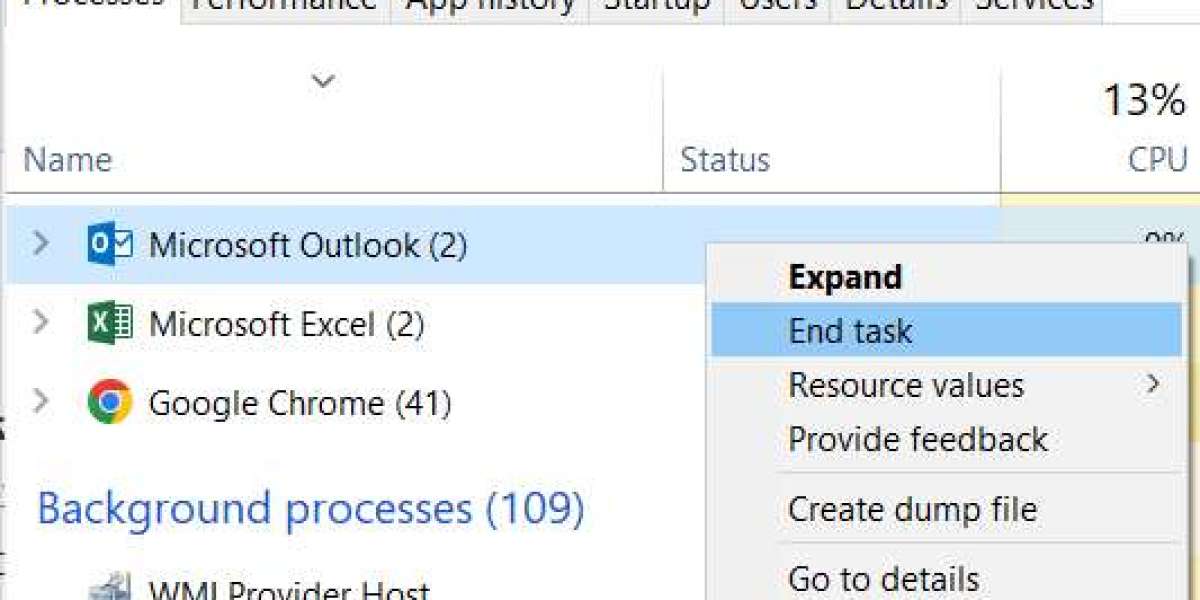
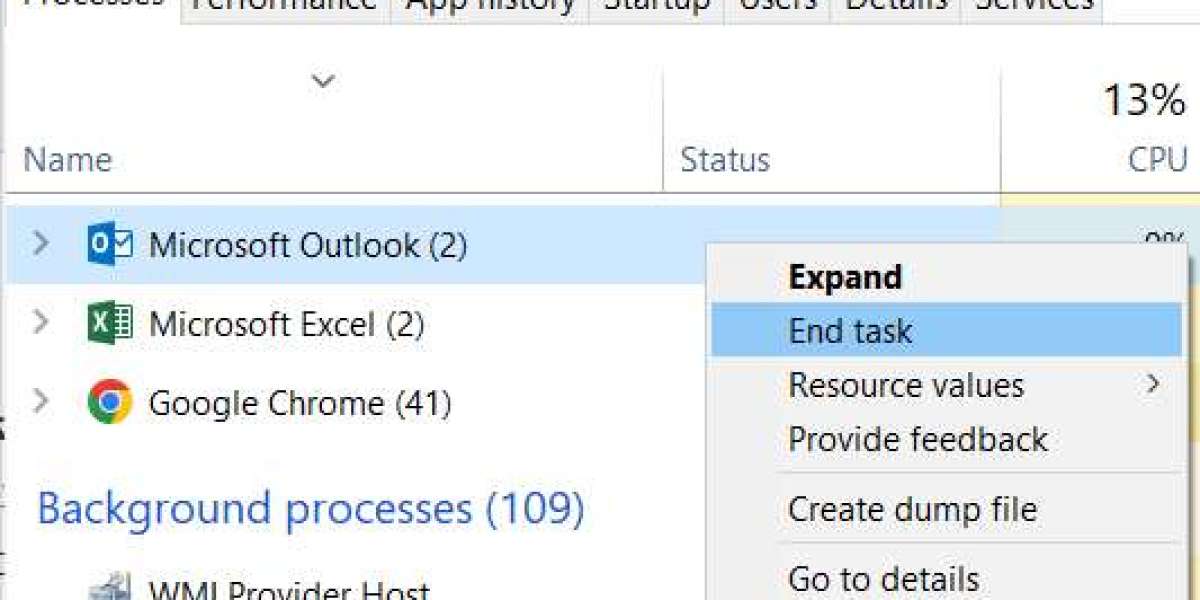
Verifying patient insurance, obtaining clinical documentation, submitting requests, and corresponding with insurers are the traditional manual phases in the healthcare prior authorization process flow. Each of these procedures takes a lot of time and is prone to mistakes, which frequently results in delays in patient care. By incorporating electronic technologies that enable real-time verification, automatic form completion, and direct submission to insurers, automation platforms streamline this process. Clinics are able to devote more time to patient care and less time to administrative duties as a result.
Prior Authorization Solutions' Advantages
Tools that monitor approvals, notify providers of missing paperwork, and even forecast possible denials are all part of contemporary prior authorization systems. Clinics can automate repetitive processes like confirming health insurance preauthorization standards or submitting pre authorization in medical billing requests by utilizing medical prior authorization software. These platforms frequently include dashboards that give a comprehensive picture of all requests, both granted and pending, allowing providers to act swiftly and decisively.
Cutting Down on Patient Care Delays
Prior authorization delays may cause surgeries and procedures to be delayed, which could have an impact on patient outcomes. Automation guarantees that requests are handled quickly when prior authorization is obtained for surgery and other crucial procedures. End-to-end pre authorization services that automatically get the required clinical data are made possible by integration with EHR systems, which lowers rejection rates and manual error. Better communication between clinics and insurers is also advantageous since automated systems may send clarifications or extra paperwork straight to the insurer when needed.
Specialized Prior Authorization Services and Outsourcing
Certain clinics decide to contract with medical prior authorization companies or prior authorization corporations to handle their prior authorization needs. These specialized suppliers successfully manage large amounts of requests by combining skilled personnel with automated technology. Clinics can save money on administrative expenses, lessen employee fatigue, and stay in compliance with insurance regulations via outsourcing. Automation guarantees a quicker, more precise prior permission for insurance and other medical services, whether it is done internally or through outsourcing.
Automation in Prior Authorization in the Future
Automation systems and prior authorization solutions are not merely a fad; they are quickly becoming the norm in contemporary healthcare. Technology can help clinics expedite approvals, increase operational effectiveness, and improve patient satisfaction by making the prior authorization process easier for providers. The industry is heading toward a future where clinical treatment takes center stage and administrative hassles are reduced as more healthcare institutions implement medical prior authorization software.