The revenue cycle, payer relationships, and patient access of a medical practice can all be seriously hampered by credentialing errors. Claims may be rejected, payments postponed, and contracts may even be terminated when provider enrollment expires if necessary documentation is not renewed on time. The good news? Practices can recover swiftly and avoid long-term harm with the correct plan and assistance from knowledgeable medical credentialing services.
1. Perform an audit of credentials immediately
Determining the extent of the lapse is the first stage in the recovery process. Examine payer contracts, CAQH profiles, board certificates, licenses, DEA registrations, and malpractice insurance. Determining whether payers are impacted and if retroactive billing is feasible is aided by an internal audit or professional credentialing services for providers.
Primary source verification, compliance gap identification, and remedial action plan development are all possible with specialized healthcare credentialing services. Quick action lowers the chance of noncompliance and minimizes income loss.
2. Get in touch with payers and ask for reinstatement.
Inform insurance networks right away if there has been a lapse and start the reactivation procedure. Requesting retroactive reinstatement is advised by several insurance credentialing organizations, particularly if services were rendered during the lapse period. If documentation is submitted on time, some payers might let claims be resubmitted.
Because they are familiar with payer-specific standards and timelines, working with seasoned insurance credentialing services or medical insurance credentialing services increases the likelihood of a quicker clearance.
3. Restart Enrollment of Providers
Practices are required to restart the provider enrollment and credentialing process in circumstances where enrollment has been terminated. This involves sending revised applications to Medicare, Medicaid, and commercial payers.
Reprocessing can be greatly accelerated by outsourcing provider enrollment or collaborating with provider enrollment services. By ensuring that applications are correct, comprehensive, and in compliance with payer criteria, professional physician credentialing services lower the likelihood of additional rejections.
Working with Medicaid credentialing specialists is particularly beneficial for government payers because Medicaid regulations differ from state to state and may call for stringent paperwork.
4. Talk about Network Participation and Hospital Privileges
Hospital connections may also be impacted by credentialing errors. Using specialized hospital credentialing services can help preserve referral networks and promptly restore compliance if hospital credentials are impacted.
In the same way, working with respectable healthcare credentialing organizations guarantees prompt correspondence with payers and accurate documentation submission in the event that network membership is compromised.
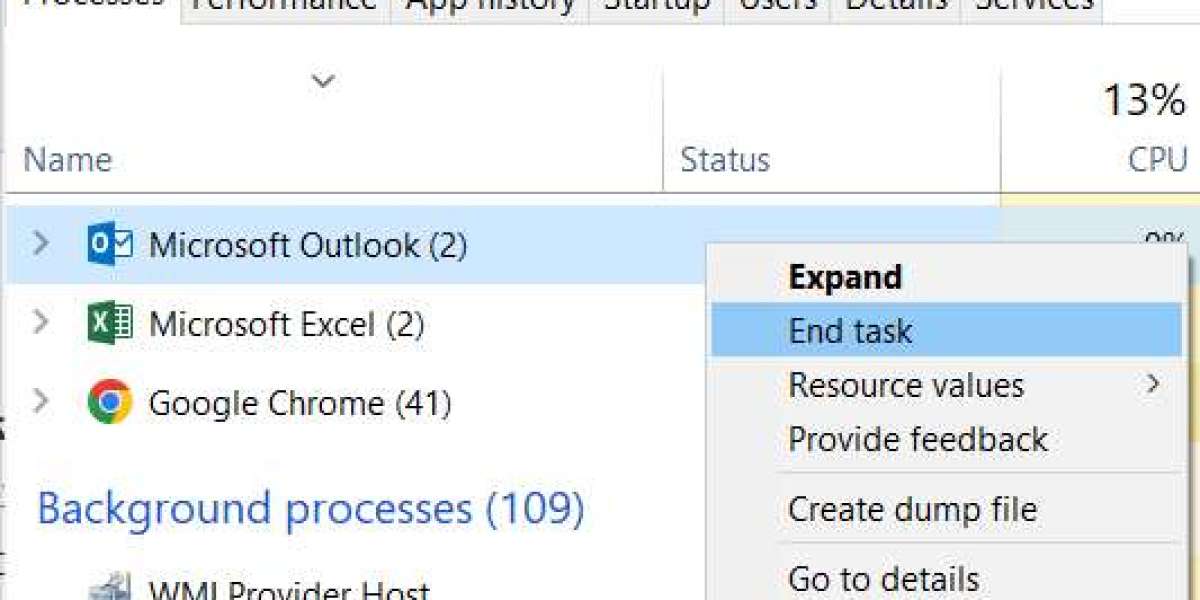
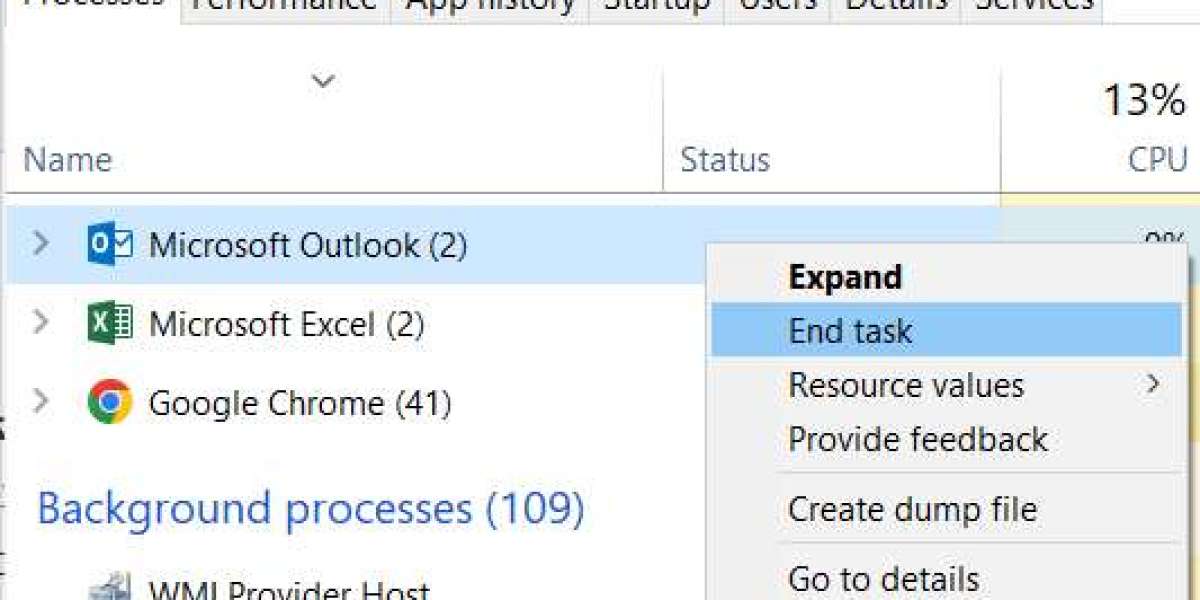
5. Make Credentialing Monitoring Systems Stronger
The key to the solution is prevention, not recovery. Manual tracking errors or a lack of supervision cause gaps in many processes. Putting in place automated monitoring systems or collaborating with top medical credentialing firms can offer:
Alerts on expiration dates
Monitoring and attestation of CAQH
Tracking applications in real time
OIG and monitoring for exclusion
Continuous management of re-credentialing
To avoid missed deadlines and enrollment problems, professional healthcare credentialing services establish organized procedures.
6. To lessen the administrative burden, outsource
Managing credentialing internally can be a daunting task for multispecialty groups and expanding firms. Selecting reputable insurance credentialing services to handle provider enrollment saves administrative burden and guarantees ongoing compliance.
In addition to managing re-enrollment, skilled credentialing services also handle revalidation, negotiate payer contracts, and offer continuing assistance to safeguard revenue streams.
Concluding remarks
Although they can be expensive, credentialing errors are recoupable. Practices can regain billing capabilities and protect future revenue by completing a comprehensive audit, reactivating payer enrollments, utilizing provider enrollment services, and collaborating with reliable healthcare credentialing organizations.
By preventing gaps through proactive management through professional medical credentialing services, clinicians may concentrate on providing high-quality patient care rather than dealing with administrative setbacks.