The use of modifiers is essential to maintaining billing accuracy and optimizing revenue in the complicated reimbursement environment of today. The correct application of modifiers can make the difference between clean claim approvals and expensive denials for healthcare companies that depend on medical billing services.
Recognizing Medical Billing Modifiers
Modifiers are two-character codes that are appended to CPT or HCPCS codes to provide more details about a service rendered. These codes are frequently alphanumeric or numeric. They provide clarification on particular situations, including bilateral services, multiple procedures, or different procedural services. Modifiers, when properly used, convey medical need and avoid miscommunications between payers and providers.
Nonetheless, one of the main causes of claim rejections is the absence or incorrectness of modifiers. Advanced medical billing services software and skilled medical billing firms are crucial in this situation.
The Effect of Modifier Accuracy on Revenue
Reimbursement levels are directly impacted by accurate modifier usage. Modifiers, for instance, can:
Avoid making mistakes when bundling
Provide evidence for increased payment for intricate treatments.
Prevent denials of duplicate claims.
Verify adherence to payer policies.
Claims for medical billing services may be underpaid, delayed, or rejected completely if the correct modifier is not applied while entering charges. Modifier-related problems are frequently identified as a primary root cause of revenue leakage by effective denial management medical billing services teams.
Outsourcing's Impact on Modifier Accuracy
In order to decrease errors and boost financial performance, many clinics decide to outsource medical billing services. Access to certified coding specialists who remain current with evolving payer policies and modifier rules is one of the main advantages of outsourcing medical billing services.
Before submitting claims, knowledgeable billing teams routinely review them to make sure:
Proper matching of modifiers
Appropriate documentation assistance
adherence to commercial payer regulations and Medicare
Modifier complexity is significantly higher for establishments like hospitals. Expert monitoring is crucial for hospital medical billing services, which must handle modifiers for surgical treatments, outpatient operations, and bundled payment scenarios.
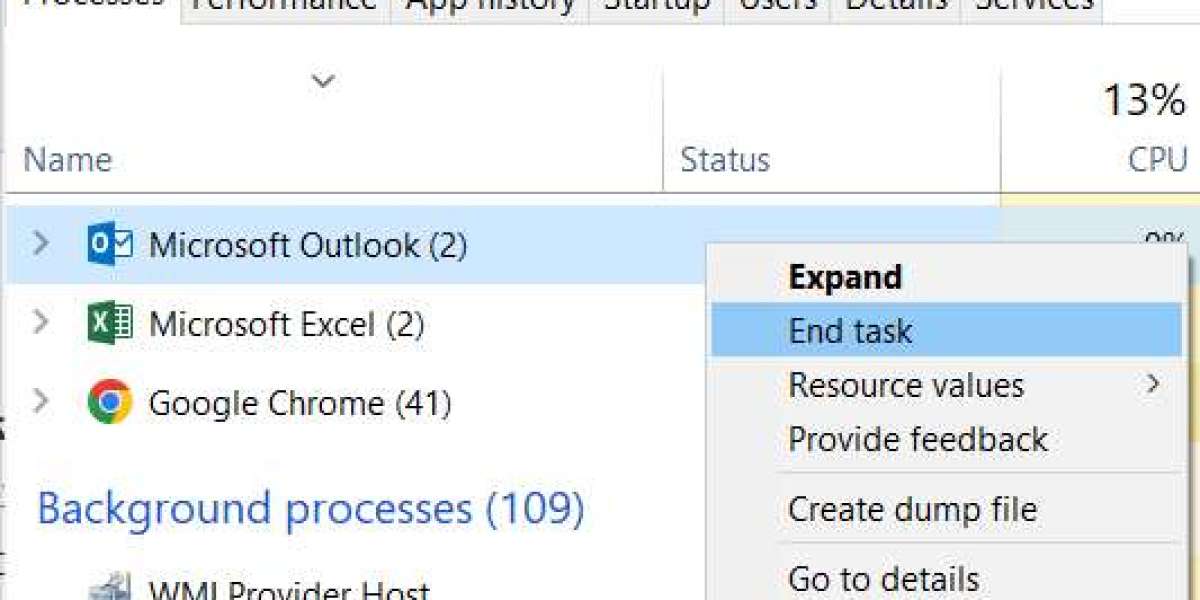
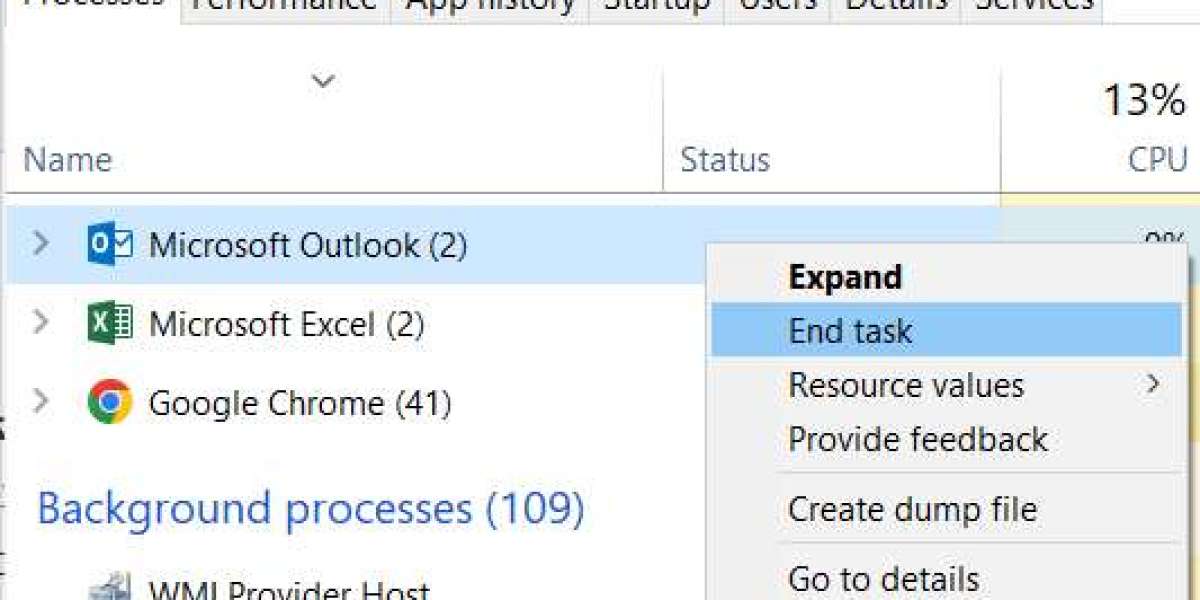
Support for Software and Technology
Automated claim scrubbing technologies are integrated with modern medical billing services software to identify missing or incorrect modifiers prior to submission. These methods improve first-pass claim acceptance rates and decrease human error.
But software is insufficient on its own. To choose the right modifier, knowledgeable billing specialists must appropriately evaluate the material. The most dependable outcomes for medical billing services for provider groups are produced by integrating technology with experienced evaluation.
Accuracy vs. Cost: A Wise Investment
The cost of medical billing services makes some physicians hesitant, but the long-term financial consequences of using the wrong modifier frequently outweigh the cost of hiring a professional billing assistant. Net revenues might be considerably lowered by denials, appeals, postponed reimbursements, and compliance issues.
Purchasing top-notch billing services guarantees:
Decreased days of accounts receivable
Higher rates of clean claims
Reduced rates of denials
Improved adherence to regulations
The Bottom Line
The use of modifiers is essential to accurate billing and is not only a technical feature. Modifiers safeguard income, lower denials, and improve overall financial performance when properly managed with the help of expert medical billing services, appropriate training, and cutting-edge technology.
Accurate modifier application is no longer optional for healthcare providers looking to maximize reimbursement and reduce compliance risks; it is now necessary for long-term success.