Insurance billing, patient safety, and quality care define and shape healthcare organizations. What many don’t see, and is just as important, is medical credentialing, which guarantees a healthcare provider’s qualification, license, and/or authorization to practice. This uncontrolled process balances safety between patients, providers, and the healthcare institution.
Why Safety is the Biggest Concern of Your Patients
The credentialing process is not just another box to check off. It consists of a lot of behind-the-scenes work including extensive verification of education and training, clinical competence, work history, as well as patient treatment history. This is the process credentialing services use to help mitigate the risk of malpractice, medical errors, or any other compliance issues.
It is imperative to work with a credentialing company. They do the primary source verification as well as the monitoring and updating of the credential file. Because of the nature of healthcare, your credentialing company will be working with an abundance of data, and not doing this will lower the quality of care that the patients receive.
Provider Enrollment = Quality Care
The provider enrollment process is just as important, if not more, as the credentialing process. This is the process that guarantees that healthcare providers will receive payment for the services that they provide. In order for this to happen, the healthcare provider must be enrolled with the insurance payer, Medicare, and Medicaid.
As part of quality patient care, the clinicians and the healthcare organizations must meet all of the requirements for provider enrollment and be accurately enrolled from private to public payer programs. This will result in reduced claim denials and seamless care for the patient.Physician and Hospital Credentialing
When physicians and hospitals utilize physician credentialing services, they learn to value clinical competence and learn about their own scope of practice. The hospitals use structured services for hospital credentialing to grant privileges, review their performances, and maintain the laws set by the regulating authorities of hospitals including their degrees of accreditation.
Large hospitals and hospital systems frequently collaborate with healthcare credential partners to simplify healthcare credentialing for complex situations, guaranteeing that every healthcare professional has met the requirements for the provision of services with the appropriate level of safety, the correct degree of quality, and the required level of compliance.
Insurance and Medicaid Credentialing
Providers must have their insurance credentialing process completed before they can treat patients. If there are mistakes or delays, patients may not be able to receive the required healthcare services. For this reason, healthcare providers who are not Medicaid providers must maintain their Medicaid credentialing process to ensure that patients who fall under the category of high-risk vulnerable populations are able to receive healthcare services that are not only timely but are also safe and compliant with the requirements of healthcare regulations.
Benefits of Outsourcing Credentialing
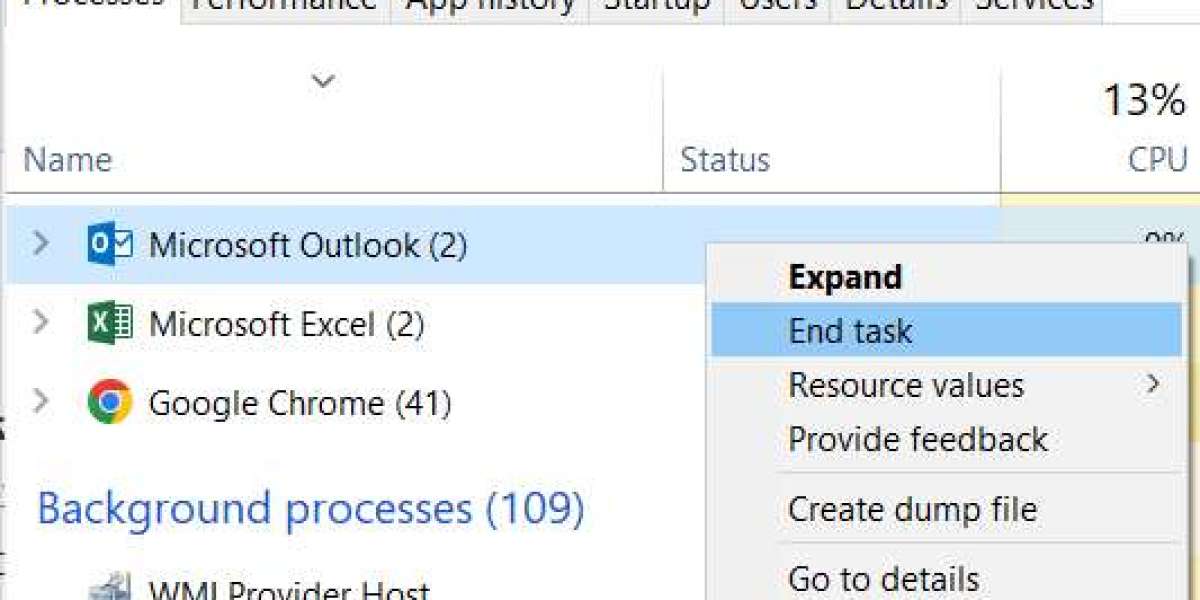
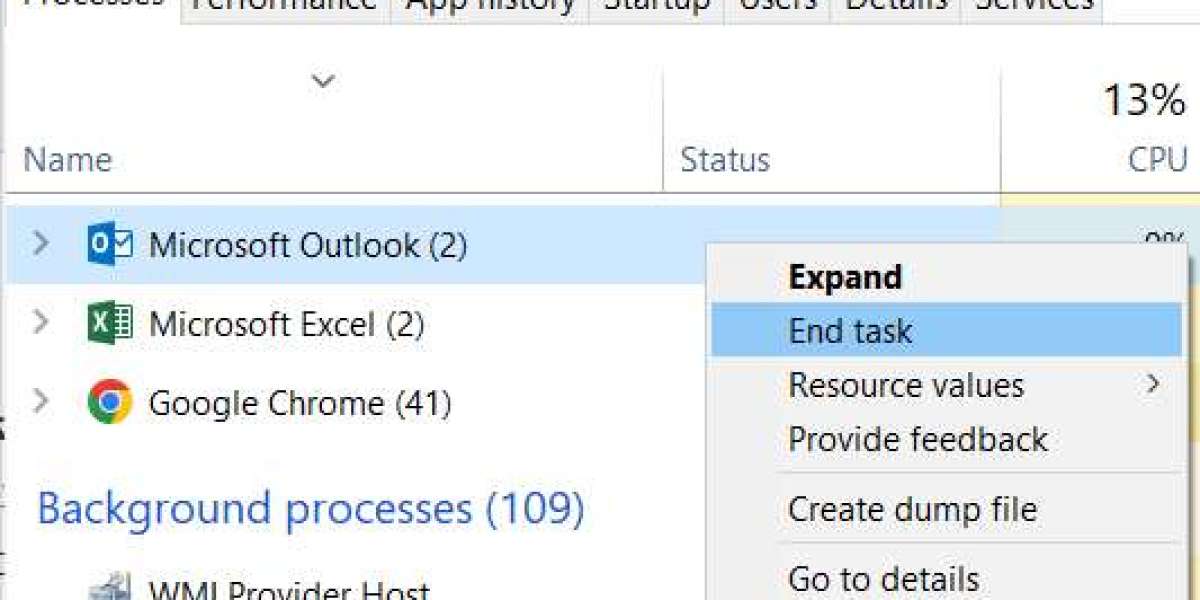
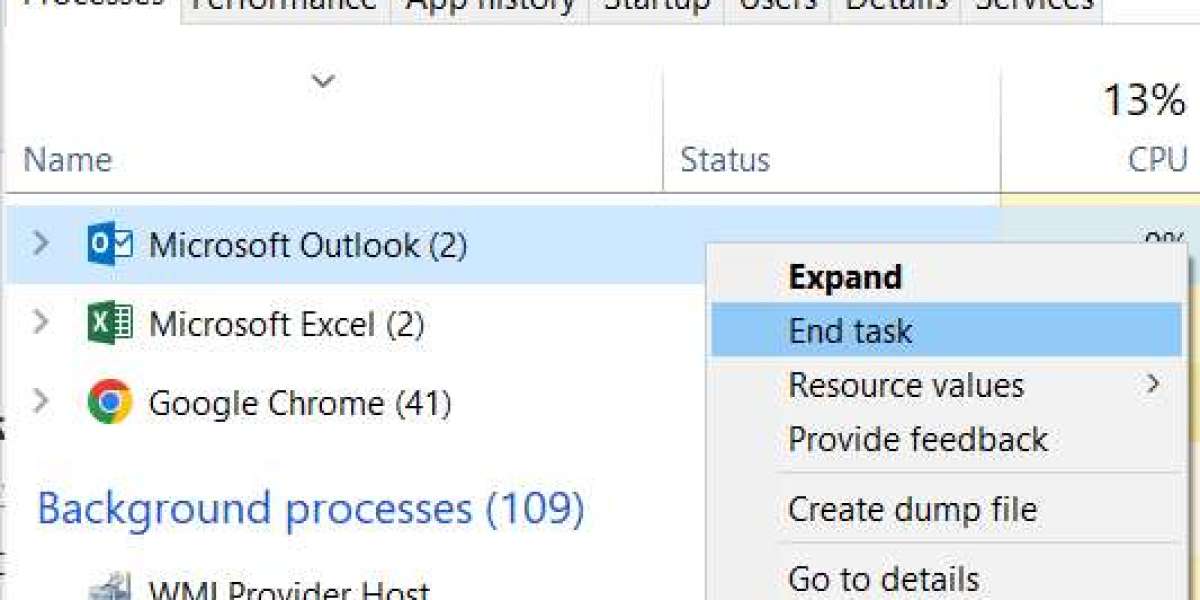
Simple automation has given many practices the opportunity to delegate the processes of provider enrollment and credentialing to partners who they trust. This has occurred as a result of improved automation. Also, the best medical credentialing companies utilize their expertise, advanced technology, and payer knowledge to increase accuracy and increase turnaround times.
Healthcare businesses can keep their focus mainly on the quality of their healthcare services instead of spending resources to become over-complex by outsourcing to experienced credentialing services and doing so removes administrative burdens and keeps them compliant with the law.
Credentialing as Quality Control
Credentialing is not done once and now it is done forever, it is done continuously and so is monitoring of the credentialing, re-credentialing, and updates to the payers, and this is to ensure that the provider is safe and is of quality throughout the provider's career. Long-term trust from patients can be obtained by maintaining compliance and supporting it with the services of credentialing.
So, What Does this Mean? Credentialing is the fiduciary safeguard to the integrity of the healthcare system. Healthcare's operational and ethical ecosystem makes it possible to provide qualified, dependable, and credentialed care to patients through provider enrollment services, hospital credentialing services, and by outsourcing to premier healthcare credentialing services.