Fundamentally, insurance claims are a big part of a business's revenue cycle. Insurance claims can be denied for a multitude of reasons, including mistakes made in submitting a coding claim, a lost or missing claim document, or an insurance claim document containing payer-specific regulations. Those in the business of providing professional medical billing services are integral to the management and settlement of claims, their work providing a means for medical professionals to recapture previously lost revenue.
Finding the Reason for Claim Denials
The first step in the appeals process is to review and analyze the relevant denial. From their experience, professional medical billing services systematically review and analyze the relevant EOBs and remittance advice. With claim denials, root causes can often be correlated with systematic and administrative errors, such as wrong patient billing information, mistakes in medical billing coding, and charge entry errors. Through careful analysis, professional billing services seek to prevent systematic and administrative errors from recurring in future claims.
Proper and Thorough Documentation
Once denial reasons are understood, medical billing specialists are tasked with gathering the relevant clinical documentation, relevant physician notes, and coding errors that need to be addressed. This step is particularly pertinent with claims for services rendered in hospitals, given the complex and interdepartmental nature of such claims. To comply with the documentation required aspects of payer-specific appeal policies, claims are carefully analyzed and corrected to optimize the prospects of approval upon appeal.
Structured Appeal Submission
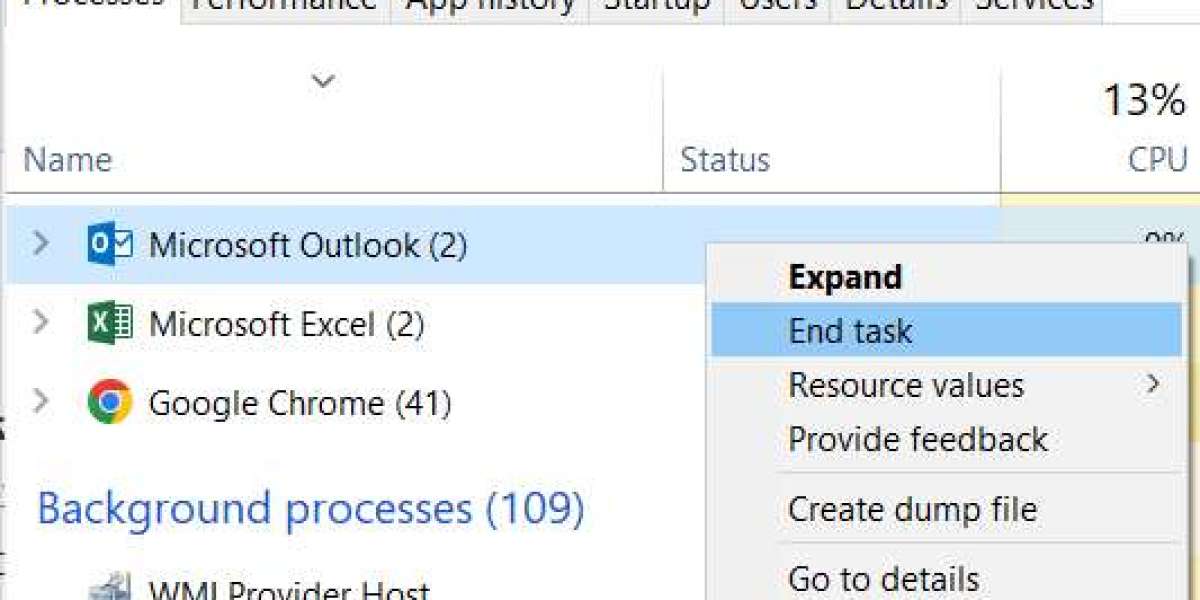
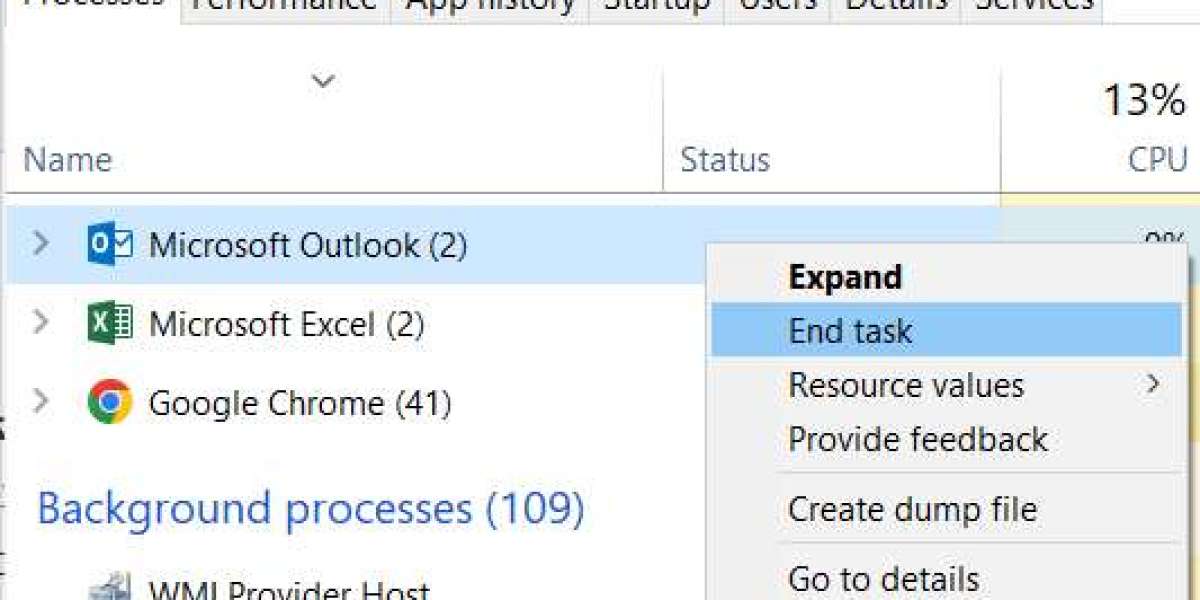
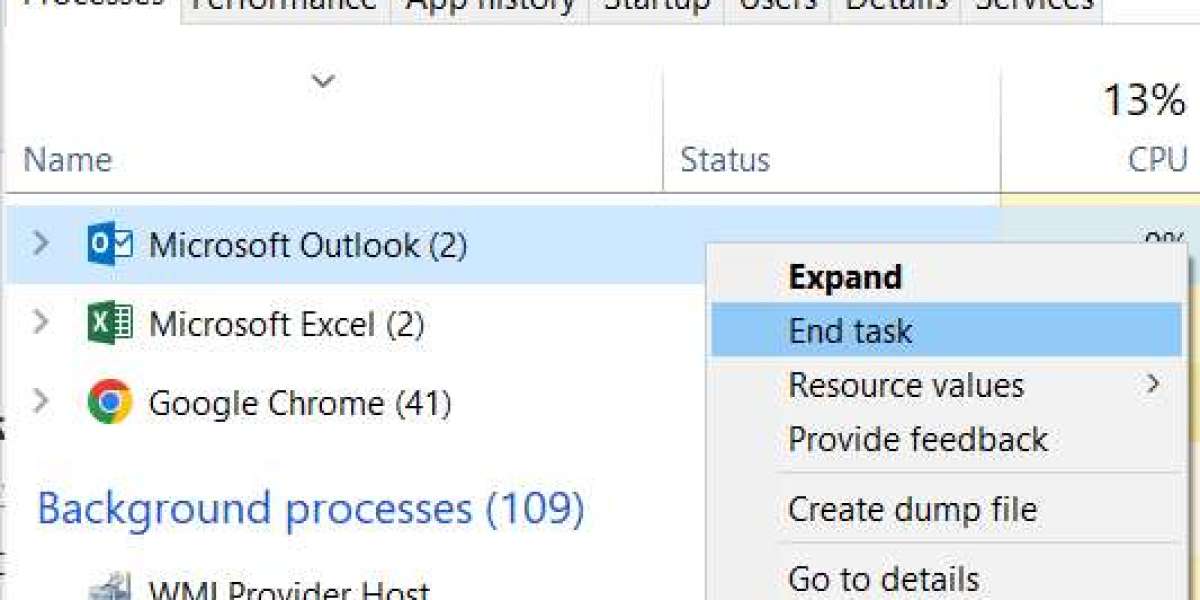
Professional services have a clear appeal workflow. Each appeal is submitted with a clear payer-specific appeal rationale and compliant medical records. It is coupled with the required timelines. Medical billing services software tracks timelines, adds documents, and checks appeal statuses so that all opportunities for repayment are documented and utilized.
Ongoing Follow-Up and Payer Engagement
Billing appeal claims are not the end of the process. Billing teams are insistent in their engagement with insurance payers regarding the claims. For this purpose, many providers find it beneficial to contract medical billing services, since internal staff will not have the time required to sustain the level of detail, engagement, and effort required to win in billing appeals.
Analysis and Reporting
There are no appeals that remain unreported. Evaluation is required for every appeal outcome, and has to be systematically documented. The best medical billing services for providers have the best appeal reporting, along with the reporting of denials and payer behavior, and appeal reporting is no exception. This allows primary care providers to improve their front-end processes (i.e., eligibility, coding, and documentation) to increase the accuracy of their reporting to payers.
Advantage of Outsourcing Medical Billing Services for Appeals
You can access greater expertise on appeals and minimize internal workload. Outsourced teams engage with payer policies and compliance on a regular basis and can obtain faster and greater monetary recoveries from appeals. Although medical billing services have a cost and it varies by provider and claim volume, winning appeals are likely to recover a lot more than what was spent on outsourcing.
The Importance of Appeals Management
Provider revenue and satisfaction hinges on successful appeals management. Regardless of whether it is a small practice or a large hospital, medical billing companies are able to ensure that denied claims are not written off too soon. Through a combination of skilled processes, technology-based workflows, and diligent follow-up, billing services convert denied claims into payments.