Introduction
Pain management today requires a deep understanding of the biological pathways behind different types of pain. Medications like Aspadol 100 mg, which contain tapentadol as the active ingredient, are designed to interact with multiple pain mechanisms. Tapentadol’s dual action—opioid receptor activation and norepinephrine reuptake inhibition—makes it an important topic for clinicians and pain researchers studying how a single agent can influence both nociceptive and neuropathic pathways.
This comprehensive blog explores the science behind tapentadol, how Aspadol 100 mg fits into clinically monitored pain therapy, and why its mechanism is relevant in conditions where pain is complex, chronic, and resistant to first-line treatments.
1. Understanding Pain: A Dual-Pathway Problem
Effective pain management begins with understanding that pain is not a single, uniform experience. Two major categories dominate modern clinical discussions:
1.1 Nociceptive Pain
This type of pain arises from tissue damage or inflammation. It is typically described as:
Sharp
Throbbing
Aching
Localized
Examples include:
Musculoskeletal injuries
Arthritis
Post-surgical discomfort
Nociceptive pain is driven by activation of nociceptors—sensory receptors signaling tissue injury.
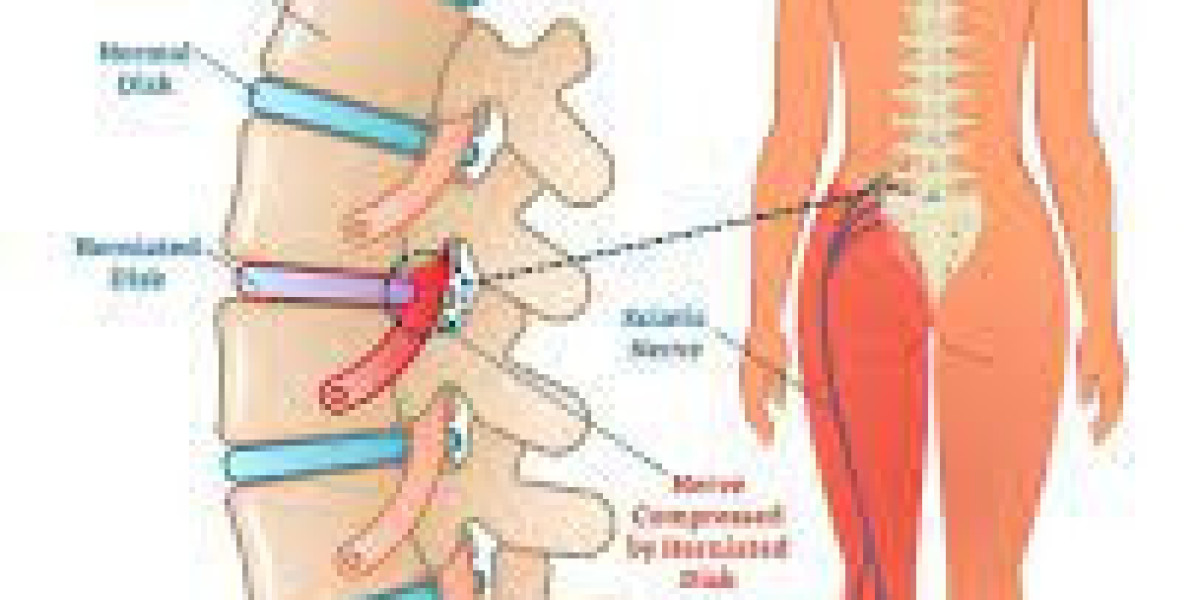
1.2 Neuropathic Pain
Neuropathic pain results from nerve injury or pathological signal processing. It may present as:
Burning
Shooting
Tingling
Electric shock-like sensations
Conditions that involve neuropathic pain include:
Diabetic neuropathy
Radiculopathy
Persistent post-surgical nerve pain
Central pain syndromes
This type of pain often responds poorly to traditional opioids alone.
1.3 Why Dual-Mechanism Analgesics Are Important
Because many chronic pain syndromes involve both nociceptive and neuropathic components simultaneously, researchers have explored medications capable of modulating multiple pathways.
Tapentadol stands out because it includes two clinically recognized mechanisms:
mu-opioid receptor (MOR) activity for nociceptive pain
norepinephrine reuptake inhibition (NRI) for neuropathic pain modulation
This dual action forms the core of how Aspadol 100 mg functions in supervised pain management.
2. Tapentadol: A Dual-Mechanism Analgesic Explained
Tapentadol’s scientific uniqueness lies in the fact that it combines:
2.1 Mu-Opioid Receptor Activation
Tapentadol activates the mu-opioid receptor (MOR), which:
Reduces ascending pain signals
Modulates perception of nociceptive pain
Influences central pain processing centers
This part of the mechanism is responsible for traditional analgesic effects often required for moderate-to-severe tissue-based pain.
2.2 Norepinephrine Reuptake Inhibition (NRI)
Tapentadol also blocks norepinephrine reuptake in the central nervous system.
Why this matters:
Norepinephrine plays a major role in descending inhibitory pathways.
These pathways suppress excessive pain signaling.
Neuropathic pain often results from failure or weakening of these inhibitory systems.
By enhancing norepinephrine activity, tapentadol supports better regulation of nerve-based pain.
2.3 Synergy: More Than the Sum of Two Mechanisms
Evidence suggests that the two mechanisms work together synergistically:
MOR activation reduces the volume of pain signals.
NRI improves the brain’s ability to dampen persistent or nerve-based signals.
This creates a broader analgesic range than either mechanism alone could produce.
3. How Aspadol 100 mg Targets Nociceptive Pain
Nociceptive pain involves the activation of pain receptors due to injury or inflammation.
3.1 MOR Activation and Nociception
Aspadol 100 mg interacts with mu-opioid receptors in:
Dorsal horn of the spinal cord
Periaqueductal gray (PAG) area
Higher brain centers
This produces:
Reduced perception of pain intensity
Lower transmission of inflammatory signals
Improved tolerance for movement and rehabilitation
3.2 Pain Situations Where This Matters
Nociceptive pain appears in:
Orthopedic injuries
Postoperative states
Rheumatic flare-ups
Acute musculoskeletal pain
Aspadol 100 mg's mechanism helps reduce the discomfort that limits physical function.
4. How Aspadol 100 mg Supports Neuropathic Pain Modulation
Neuropathic pain is more complex because it arises from dysfunctional nerve pathways. Traditional opioids have limited success here.
4.1 Tapentadol’s NRI Mechanism
By inhibiting norepinephrine reuptake, Aspadol 100 mg increases synaptic norepinephrine levels.
This leads to:
Strengthened descending inhibitory pathways
Stabilization of neural signaling
Reduced central sensitization
Improved nerve pain modulation
4.2 Neuropathic Symptoms Addressed
The enhanced inhibition can reduce painful sensations such as:
Burning
Electric shocks
Tingling
Radiating pain
Hypersensitivity
This makes tapentadol scientifically relevant for mixed nociceptive-neuropathic conditions.
5. Conditions Where Mixed Pain Is Common
Clinicians frequently encounter cases where both pain types coexist. Examples include:
5.1 Chronic Low Back Pain With Radiculopathy
Combines:
Inflammatory tissue pain
Nerve compression symptoms
5.2 Osteoarthritis With Central Sensitization
Chronic joint disease often evolves into mixed pain.
5.3 Post-Surgical Pain With Nerve Involvement
Especially after spine, joint, or abdominal surgery.
5.4 Diabetic Neuropathy With Musculoskeletal Pain
Multiple systems become involved.
5.5 Trauma Leading to Persistent Mixed Pain
Nerve trauma plus musculoskeletal injury.
In such complex scenarios, the scientific concept behind Aspadol 100 mg’s dual mechanism provides insight into why some clinicians explore dual-pathway analgesics.
6. The Science of Pain Pathways: Why Dual Treatment Matters
The human pain system involves two major networks:
6.1 Ascending Pathways
Carry pain signals from the body to the brain.
6.2 Descending Pathways
Send signals from the brain to suppress pain.
In many chronic pain states, both pathways malfunction simultaneously:
Ascending signals become exaggerated.
Descending inhibitory controls become weaker.
Tapentadol helps by:
Calming ascending signals (MOR action)
Strengthening descending inhibition (NRI action)
This dual approach aligns with modern pain science theories such as central sensitization and maladaptive neuroplasticity.
7. Functional Outcomes Associated With Tapentadol Use (Educational Overview)
Clinical observations and general research insights suggest that dual-mechanism analgesics may contribute to:
7.1 Improved participation in physical therapy
Better pain control often allows patients to engage more consistently in rehabilitation.
7.2 Enhanced mobility and daily function
Pain reduction can support:
Walking
Occupational tasks
Self-care
Sleep improvement
7.3 Reduced neuropathic pain flare-ups
Enhanced NE activity may dampen nerve hyperexcitability.
7.4 Lower GI side-effect burden compared with some traditional opioids
This may support better adherence.
7.5 Better tolerability for patients with mixed pain
By targeting both components simultaneously.
These outcomes depend on individualized clinical assessment and careful monitoring.
8. Integrating Aspadol 100 mg Into Multimodal Pain Strategies
Modern pain guidelines emphasize multimodal approaches.
8.1 Physical Rehabilitation
Medication helps facilitate:
Range-of-motion work
Strengthening
Core stability training
Functional conditioning
8.2 Psychological Interventions
Chronic pain often involves emotional and cognitive factors.
Therapies include:
CBT
Pain acceptance strategies
Relaxation techniques
8.3 Pharmacological Combinations Under Clinical Guidance
Tapentadol may be paired with:
Neuropathic agents
Anti-inflammatory drugs
Muscle relaxants
8.4 Lifestyle Optimization
Includes:
Sleep hygiene
Anti-inflammatory diet
Stress regulation
Medication becomes one piece, not the entire solution.
9. Important Safety and Clinical Monitoring Considerations
Because Aspadol 100 mg acts on the central nervous system, it must be used under medical supervision.
9.1 Clinical Screening
Providers evaluate:
Respiratory function
Sedation risk
Comorbidities
Drug interactions
Past analgesic response
9.2 Ongoing Monitoring
This includes:
Pain scores
Functional improvements
Possible side effects
Treatment goals
9.3 Using the Lowest Effective Dose
Dose adjustments depend on clinical evaluation.
9.4 Responsible Opioid Stewardship Principles
Modern guidelines emphasize:
Regular reassessment
Avoiding unnecessary long-term continuation
Considering tapering when appropriate
10. Case Example (Educational & Fictional)
Scenario
A 48-year-old patient experiences chronic lumbar radiculopathy and persistent musculoskeletal pain following an accident. They describe:
Burning leg pain (neuropathic)
Deep back ache (nociceptive)
Difficulty sleeping
Limited physical therapy participation
Clinicians determine that dual-mechanism analgesia may support rehabilitation.
Outcomes Over Clinical Monitoring
After supervised treatment:
Nerve pain flare-ups decrease
Mobility improves
The patient participates more actively in therapy
Sedation is monitored and managed
Pain scores stabilize
This example illustrates how dual-pathway modulation can influence functional recovery.
11. Tapentadol Research Trends and Future Perspectives
Current pain research explores:
11.1 Expanded understanding of dual-mechanism analgesics
How they differ from traditional opioids.
11.2 Precision pain medicine
Matching medication type to pain phenotype.
11.3 Neuropathic pain biomarkers
Identifying which patients benefit most from NRI components.
11.4 Improved integrated treatment pathways
Merging medication, digital therapeutics, and rehabilitation.
11.5 Ongoing focus on opioid stewardship
Balancing analgesia with long-term safety.
Conclusion
Aspadol 100 mg, containing tapentadol, offers an example of how a dual-mechanism analgesic can target both nociceptive and neuropathic pain pathways. Its MOR activity addresses tissue-based pain, while its NRI action supports descending inhibitory systems that are crucial for neuropathic pain modulation. These scientific mechanisms provide important insights into why such medications may be evaluated in clinically complex pain situations.
However, tapentadol must always be used under professional supervision, as part of a multimodal approach that includes physical rehabilitation, psychological support, lifestyle management, and ongoing clinical monitoring. Understanding its science helps both clinicians and patients appreciate the complexity of treating chronic pain in a responsible, evidence-driven manner.
Frequently Asked Questions (FAQs)
1. What makes Aspadol 100 mg different from traditional opioids?
Its dual mechanism combines mu-opioid receptor activation with norepinephrine reuptake inhibition, targeting both nociceptive and neuropathic pain pathways.
2. Does Aspadol 100 mg help with nerve pain?
Tapentadol’s norepinephrine reuptake inhibition may support neuropathic pain modulation, depending on clinical factors.
3. Is Aspadol 100 mg suitable for all types of chronic pain?
Not necessarily; clinicians evaluate patient history, comorbidities, and pain characteristics before deciding.
4. Can Aspadol 100 mg be used long term?
Long-term use depends on ongoing clinical evaluation and evidence-based prescribing guidelines.
5. How does tapentadol improve pain functionally?
By reducing pain intensity and stabilizing nerve signaling, patients may engage more effectively in rehabilitation.
6. Is Aspadol 100 mg part of multimodal pain therapy?
Yes, it is typically combined with physical therapy, psychological strategies, and lifestyle modifications.
7. What precautions are necessary?
Professional supervision, monitoring for side effects, avoiding interactions, and ensuring safe use.