Transforming Health Insurance Administration in the Modern Era
The healthcare industry across the Middle East has experienced significant advancement in recent years, particularly in how health insurance claims are managed and processed. Third-party administrators have emerged as essential intermediaries who ensure smooth coordination between insurance carriers, medical facilities, and policyholders. These specialized entities handle the intricate details of claims processing, provider network management, and member services that require dedicated expertise and sophisticated technology infrastructure. The demand for professional administration services continues growing as insurance portfolios expand and healthcare delivery becomes increasingly complex across the region.
Seamless Healthcare Access via the Lifeline Network
The lifeline network serves as a comprehensive healthcare ecosystem connecting insured members with quality medical providers throughout the Gulf region. This extensive infrastructure enables policyholders to access medical services without immediate financial burden through cashless facility arrangements. By establishing relationships with hundreds of hospitals, clinics, pharmacies, and diagnostic centers, the network ensures convenient healthcare access across multiple locations. Members benefit from simplified procedures where pre-authorization and claim settlement happen behind the scenes through digital platforms. Real-time connectivity between providers and administrators facilitates instant verification of coverage, reducing wait times and administrative friction at point of service. The network's strength lies in its careful selection of healthcare partners based on quality standards, service excellence, and geographic distribution to serve diverse member populations effectively.
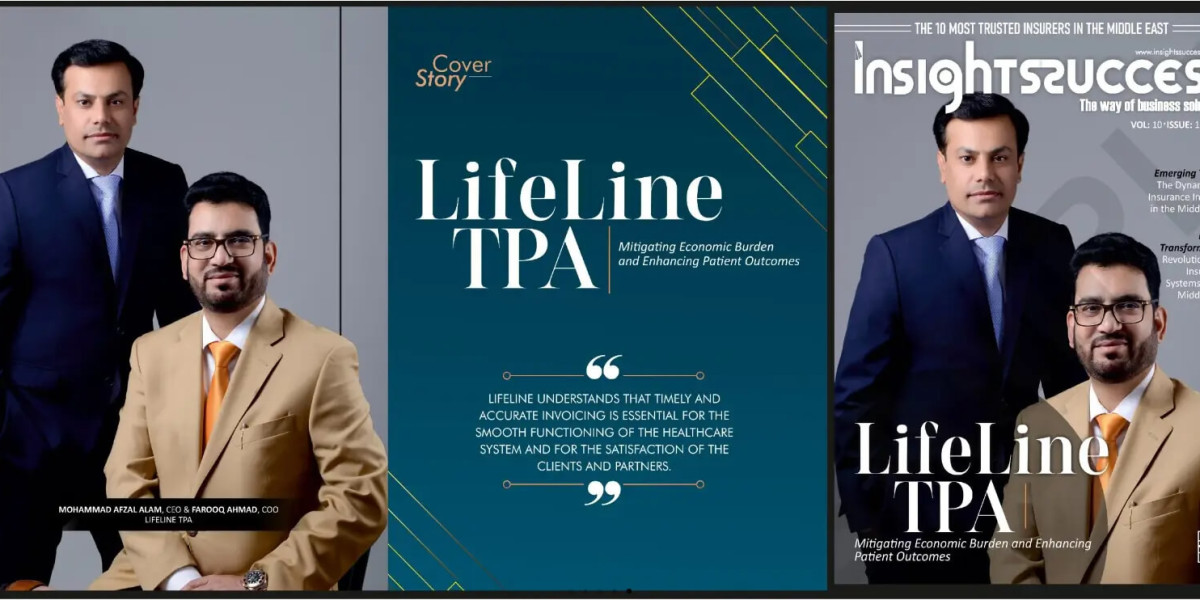
Professional Healthcare Management by Khat Al Haya Management of Health Insurance Claims LLC
Established in 2015, Khat Al Haya Management of Health Insurance Claims LLC operates as a dedicated third-party administrator serving markets across the United Arab Emirates, Oman, and Turkey. The organization specializes in comprehensive claims administration including processing, settlement, reconciliation, documentation management, and policy maintenance for various insurance partners. Through deployment of advanced adjudication systems incorporating thousands of business rules, the company achieves automated processing for more than eighty percent of incoming claims. This automation significantly enhances efficiency while maintaining accuracy and consistency in applying policy terms. The administrative platform supports multiple insurance products ranging from individual and family plans to large group and corporate schemes. Strong relationships with insurance carriers and reinsurance companies enable effective risk management and financial coordination throughout the claims lifecycle.
Characteristics That Define the Best TPA in UAE
Organizations seeking to identify the best TPA in UAE should evaluate several critical performance dimensions including technological sophistication, network quality, service responsiveness, and operational integrity. Premier third-party administrators demonstrate commitment to excellence through investment in modern claims management systems, comprehensive fraud prevention programs, and responsive customer support infrastructure. Superior service delivery manifests in quick turnaround times for claim decisions, accurate payment processing, and proactive communication with all stakeholders. Top-tier TPAs maintain robust quality assurance programs that monitor provider performance, audit claim patterns, and ensure compliance with regulatory requirements. Data analytics capabilities enable these organizations to provide insurance partners with actionable intelligence on utilization trends, cost drivers, and opportunities for program optimization. Professional development initiatives ensure staff members possess current knowledge of medical terminology, coding systems, and industry regulations essential for informed decision-making.
Comprehensive Service Portfolio Through Lifeline TPA
Lifeline TPA delivers integrated administration services designed to meet diverse client requirements across individual, family, group, and corporate insurance segments. The organization's wellness initiatives promote proactive health management through preventive care programs, health screenings, and lifestyle counseling services. Digital engagement tools including mobile applications and web portals empower members with self-service capabilities for policy information access, claims tracking, and provider location services. Emergency medical assistance protocols ensure immediate support during critical situations with coordinated authorization processes that prioritize patient care. Value-added services such as second medical opinion programs provide members with additional expert consultation on complex medical conditions or treatment recommendations. New member orientation programs familiarize policyholders with benefit structures, utilization procedures, and available support resources. The customer care infrastructure operates continuously through dedicated call centers staffed with multilingual representatives trained to address inquiries promptly and accurately.
Developing Strong Collaborative Relationships
Successful healthcare administration depends fundamentally on cultivating productive partnerships across the healthcare value chain. Collaboration with insurance companies focuses on shared objectives of member satisfaction, cost containment, and quality improvement. Provider partnerships emphasize mutual respect, fair contracting terms, and efficient operational workflows that benefit both medical facilities and patients. Network development extends beyond numerical growth to include rigorous credentialing processes, ongoing performance monitoring, and regular quality assessments. The organization maintains contractual arrangements with diverse healthcare providers throughout the GCC region, offering members extensive choice in accessing medical services. These relationships thrive through transparent communication, timely financial settlements, and collaborative problem-solving approaches. Regular engagement forums with insurance partners facilitate continuous improvement through feedback exchange, process refinement, and joint planning for emerging challenges.
Leveraging Technology for Operational Efficiency
Contemporary healthcare administration relies extensively on integrated technology platforms that streamline complex workflows and enhance decision accuracy. Sophisticated claims engines apply multifaceted rule sets to evaluate coverage eligibility, determine benefit applicability, and calculate appropriate reimbursements automatically. Electronic connectivity enables real-time information exchange between healthcare providers, administrators, and insurance carriers. Advanced analytics platforms process large datasets to identify patterns, detect anomalies, and generate insights that drive strategic decisions. Member-facing digital channels reduce dependency on traditional support channels while improving convenience and satisfaction. Cloud-based infrastructure ensures system reliability, scalability, and security for sensitive health information. Ongoing technology investments focus on emerging capabilities like artificial intelligence for pattern recognition, predictive modeling for risk assessment, and enhanced cybersecurity measures to protect stakeholder data.
Upholding Principles of Transparency and Trust
Transparent operations form the foundation of credible healthcare administration that earns stakeholder confidence. Clear articulation of policy terms, coverage parameters, and claims procedures helps members navigate their benefits effectively. Honest communication regarding claim decisions, including detailed explanations for denials, maintains organizational credibility. Open dialogue with healthcare providers about documentation requirements and reimbursement methodologies fosters productive working relationships. Comprehensive reporting to insurance partners demonstrates accountability and facilitates objective performance assessment. Structured feedback mechanisms including member surveys and grievance procedures drive organizational learning and service enhancement. The administrative approach balances efficiency with empathy, recognizing that behind every claim lies a person seeking healthcare support. This human-centered perspective combined with operational excellence creates lasting relationships built on reliability and mutual respect.
Preparing for Healthcare's Evolving Landscape
The healthcare sector continues transforming through regulatory evolution, technological innovation, and changing consumer preferences. Progressive third-party administrators anticipate these shifts by investing in next-generation capabilities including artificial intelligence for enhanced automation, blockchain technology for secure data management, and telehealth integration for expanded service delivery options. Adaptation to value-based care frameworks emphasizes health outcomes and preventive services over transaction volume. Sustainability considerations increasingly influence operational decisions from digital documentation to energy-efficient facilities. Organizations that proactively develop future-ready capabilities position themselves as industry leaders capable of navigating complexity and delivering consistent value. Through strategic foresight, continuous innovation, and steadfast dedication to service excellence, professional healthcare administrators contribute meaningfully to the fundamental goal of accessible, affordable, quality healthcare throughout the communities they serve.